What is Canine Leptospirosis?
Leptospirosis is an infectious disease caused by a bacterium called Leptospira. Infection often causes serious damage to the kidney and liver, and can be fatal in severe cases. The organism is transmitted in the urine of infected animals and can survive in the environment for long periods of time, especially in warm stagnant water or moist soil. Wild animals, including the skunk, raccoon, opossum, rat, wolf, and deer, are an important source of infection.
How are dogs infected?
Most dogs are infected by direct contact with infected urine, or by contact with water or soil contaminated with infected urine. Leptospira can penetrate the lining of the nose, mouth and eyelid, and can also enter the body through scratches or open sores on the skin.
What happens then?
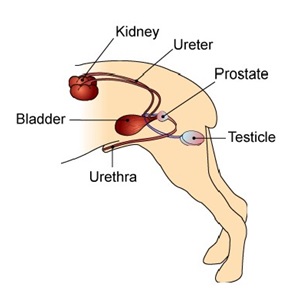
Once inside the body, the organisms replicate quickly in the bloodstream before moving into the tissues, especially the liver and kidney, where they cause serious damage.
About eight to ten days after infection, the dog's immune system responds to the infection and produces antibodies that quickly clear the Leptospira from the blood. However, in spite of this immune response, some bacteria are able to survive in the kidney, resulting in long-term infection and ongoing shedding of organisms in the urine. Dogs that have recovered but that still carry Leptospira in their kidneys are said to be in the 'carrier state'.
What are the signs of leptospirosis?
The signs of illness can be variable. Most commonly, an acute infection with Leptospira causes a severe disease that can be rapidly progressive; in some cases, it can be fatal. In other dogs, illness is mild and the infection may be present for long periods, or may even go unnoticed.
The most common signs of acute leptospirosis are lethargy, depression, loss of appetite, vomiting, fever, and increased thirst and urination. The dog may develop jaundice, which shows as a yellow tinge to the lining of the mouth or the whites of the eyes. Illness typically develops quickly, and dogs can become very sick within just a few days.
How is leptospirosis diagnosed?
Initial screening tests usually include a Complete Blood Count or CBC, a biochemical profile, and a urinalysis. (See handouts for "CBC", "Biochemistry", and "Urinalysis"). The most common test findings are:
CBC: increased white blood cell count, low platelet count, and sometimes anemia.
Biochemistry: marked elevations in kidney and/or liver enzymes, and altered electrolytes (sodium, chloride, phosphorous, potassium).
Urinalysis: dilute urine, positive for protein, and evidence of inflammation and kidney damage.
What definitive tests are available to diagnose Leptospirosis?
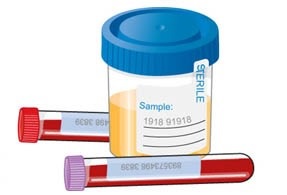
If leptospirosis infection is suspected based on initial testing, definitive testing is needed to confirm the diagnosis. There are several tests for this purpose, but the most common and readily available tests are the DNA-PCR test (See handout on DNA-PCR) and a test called the Microscopic Agglutination test. These two tests are complementary and both are often performed on the same patient.
DNA-PCR Test: This is a rapid method for detecting the DNA of Leptospira bacteria in a sample, and can be performed on whole blood and/or urine. Urine is the preferred sample because the bacteria are typically present in large numbers and therefore are more readily detected.
This is an excellent test, but it must be done before the dog is given antibiotics because Leptospira disappear from the urine very quickly once antibiotics are given. The DNA-PCR test is most useful in the early stages of acute disease, when large numbers of organisms are being passed in the urine. Dogs that have been sick for a long time, or that have mild signs, may not be passing enough bacteria for the test to detect.
It is important to remember that even when infection is present, the DNA-PCR test can be negative for a variety of reasons, and a negative result does not rule out infection. If leptospirosis is still considered a possible cause for illness, further testing will be needed to confirm infection. This usually means performing the Microscopic Agglutination test.
Microscopic Agglutination Test: This is the standard test for diagnosing leptospirosis, and is designed to detect the presence of antibodies against Leptospira in the dog's blood. If the level of antibodies (called a "titer") is high enough, then infection is confirmed.
This is an excellent test, but it may take several days to get results back from the laboratory, and sometimes a second test, taken later in the course of disease (called a convalescent sample), is needed to confirm infection. Test results can be inconclusive if the patient has been previously vaccinated for leptospirosis, or if treatment with antibiotics was started very early in the course of disease (before the immune system had time to respond to infection).

Can leptospirosis be treated?
Yes. Antibiotic therapy is usually highly effective in treating leptospirosis, and many dogs respond quickly once antibiotics are given. There are two phases of treatment. The first phase treats the acute infection, and the second clears long-term residual infection called the "carrier state". Your veterinarian will discuss the details of treatment with you.
Leptospirosis infection can cause extensive damage to the kidney or liver. In these cases, hospitalization for aggressive fluid therapy and other medical management is necessary to treat the resulting kidney or liver failure. The prognosis in these cases is more guarded, but recovery is still possible. Unfortunately, in some cases an overwhelming infection causes irreversible damage, resulting in rapid deterioration and death in spite of the appropriate aggressive treatment.
Can people catch leptospirosis from dogs?
Yes. Leptospirosis is a 'zoonotic disease', which means it can spread from dogs to people (or vice versa). Transmission usually occurs by direct contact with infected urine, and pet owners and veterinary staff should avoid getting infected urine in their eyes, nose, or mouth, or in open skin sores. Careful disposal of soiled bedding and thorough disinfection of contaminated areas is recommended. Any person feeling unwell after exposure to an infected dog should seek medical attention.
This client information sheet is based on material written by: Kristiina Ruotsalo, DVM, DVSc, ACVP & Margo S. Tant, BSc, DVM, DVSc © Copyright 2009 Lifelearn Inc. Used and/or modified with permission under license.







